People in Washington and across the country often want nothing more than to help their friends, family, and community members heal and recover from problematic substance use. But many do not know where to start.
With 16.5% of the U.S. population struggling with an substance use disorder, chances are you know someone who could use some support. The compounding circumstances of COVID-19 relief dying down, the housing crisis, and new altered and more deadly fentanyl being found in street drugs, makes offering effective and compassionate support even more critical.
Amber Frymier, a medical provider at Evergreen Treatment Services’ Seattle Clinic, shared some of the key things people should know when supporting those with an opioid use disorder.
For people in recovery, Amber stresses that friends and family must keep an open mind about what someone’s recovery journey can look like. “Everyone has different backgrounds and life experiences. This is going to change their story of substance use,” she shares. “It is important to not compare one person’s journey to another’s.”
The road to recovery is not linear, and sometimes despite their best efforts, people use again. This doesn’t mean the recovery journey is over. Amber encourages people to meet recovering patients where they are, in addition to learning the signs of escalating opioid use, knowing when to call 911, and more. “Getting people through recovery is going to take a lot of time,” Amber says. “Try to understand and learn where a person is in their recovery journey and understand that this will fluctuate and change as time moves on.”
For many concerned friends and family members, their loved ones are currently using drugs in a way that is harmful to themselves and others. Amber shared that often, family members and friends can judge their loved ones and their drug use. Instead, she encourages them to reframe their thinking around substance use disorders. “Addiction and opioid use disorders are chronic health challenges,” she shares. “It is something that has flare ups and remissions and needs to be identified and managed as such.”
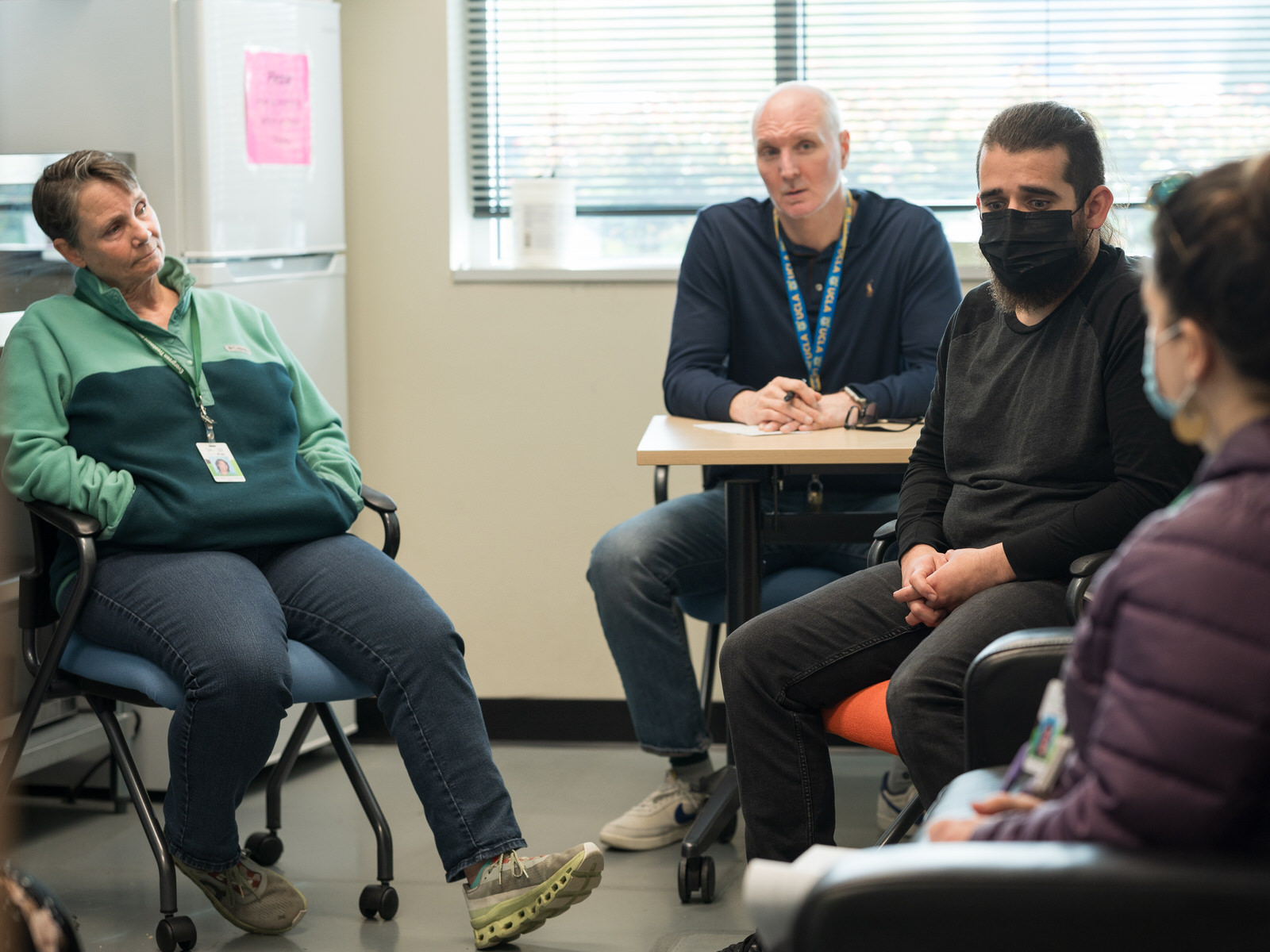
Amber emphasized that maintaining relationships with loved ones and providing emotional support and encouragement—while often challenging—can make a dramatic difference in a person’s recovery journey. Addressing the mental health side of substance use is so important that ETS provides options for group therapy and counseling to their patients to better support their emotional and mental health needs.
Above all, Amber stresses that keeping loved ones physically safe and alive takes precedence. “You can’t support and enjoy a relationship with your family member if they’re no longer here.”
For community members wanting to offer support, Amber recommends carrying Narcan. Narcan is the most common brand of naloxone, a medication used to reverse opioid overdose in an emergency. Amber encourages community members to get training to use Narcan, especially if you are a drug user or are frequently in spaces where people use drugs. ETS clients can pick up free Narcan at ETS facilities or Seattle & King County Public Health. They can also purchase it from retail pharmacies.
Additionally, Amber encourages family and friends to try motivational interviewing to understand why people use. Amber provides example questions such as: What does this medication do for you? Has it impacted your life in any negative or positive way? Do you ever think about entering treatment? These open-ended questions can help people engage with their substance use in a different way. For those asking the questions, understanding where people are in their substance use or recovery journeys, helps to better support people and refer them to resources. Learn how ETS applies motivational interviewing with our program participants in this blog.
Amber envisions a future where medications for opioid use disorders will become more accessible for providers to prescribe and people to use. Additionally, she hopes that clients can begin receiving treatment as soon as they seek it instead of being referred, alleviating some of the barriers that people seeking recovery currently face.
Everyone can recover. It is up to communities to provide all the possible paths of recovery and support for people to move forward when they’re ready. “There’s a way to help everyone, we just have to find their way and work on their timeline,” Amber says. “Keep checking in with people and keep caring, and they’ll let you know when they’re ready for a change.”




